Post Injury Confidence
Post Injury Confidence from BIOMechaniks on Vimeo.
Quality of movement should always be your main priority. However, sometimes you have to just let individuals move
Posted on March 29, 2016 | PermalinkAthletic Stability
Athletic Stability from BIOMechaniks on Vimeo.
Here we are working on control after explosive movements...many injuries occur upon deceleration...
Posted on March 21, 2016 | PermalinkKettlebell Deadlift
Kettlebell Deadlift from BIOMechaniks on Vimeo.
Kettlebell Deadlift
Posted on February 17, 2016 | Permalink#WorkoutWednesday
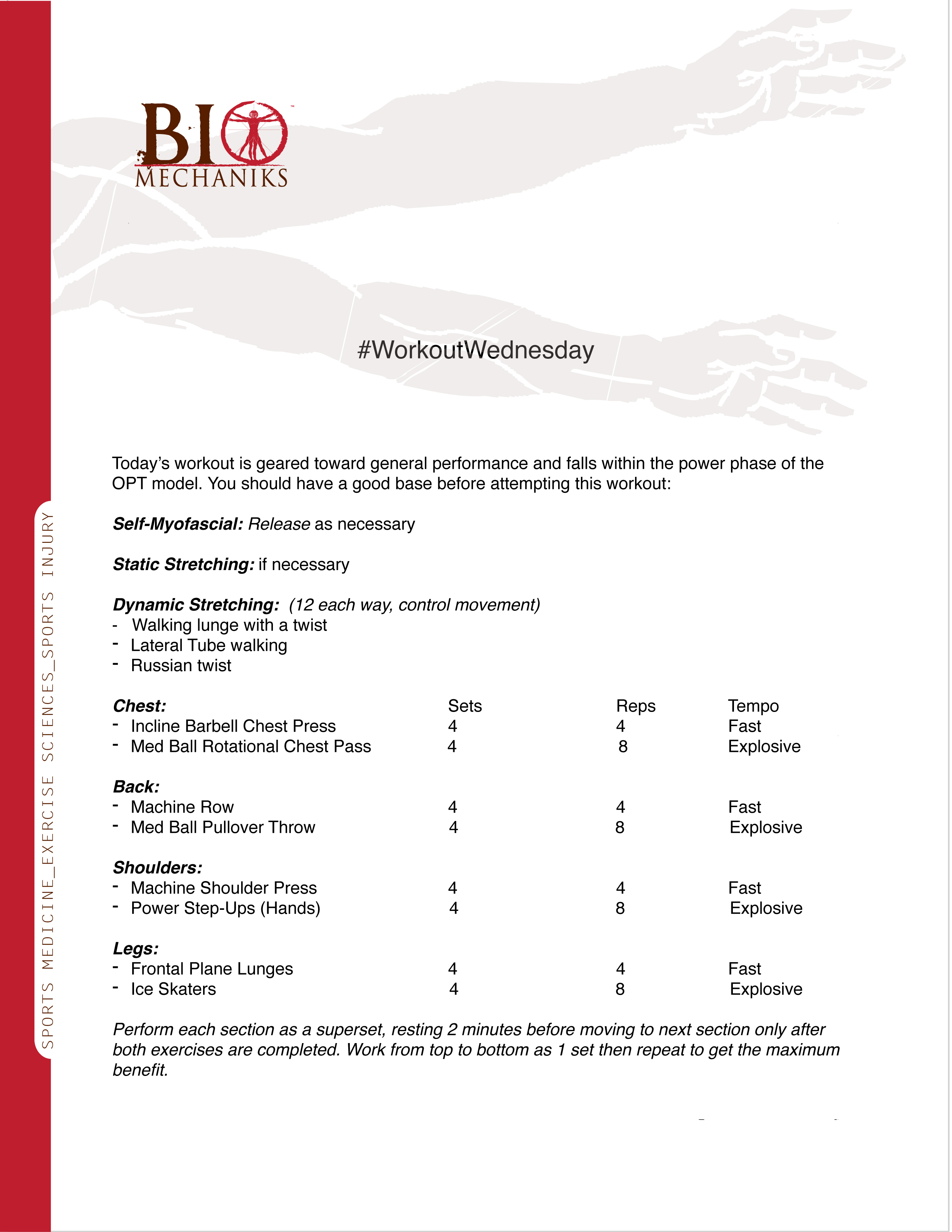
#WorkoutWednesday
Perform each section as a superset, resting 2 minutes before moving to next section only after both exercises are completed. Work from top to bottom as 1 set then repeat to get the maximum benefit.
Posted on October 8, 2014 | PermalinkGet Up, Get Out, & Get Something
Ever here someone say "if you don't use it, you lose it"? Well this is very true when it comes to human movement. Leading a sedentary life only will subject you coming closer to developing movement issues later down the road. For example, let's say you sit at a desk for 8 hours/day and you do not perform any physical activity outside of your work environment (in which you sit for 8 hours/day). Sitting for prolonged periods places the hip flexors in a shortened position for an extended period of time, thus inhibiting the glutes when you stand because your pelvis is rotated to the front (anterior pelvic tilt) as a result of your hip flexors being tight.
Now you decide that you want to do a "from couch to 5k" program to get your active lifestyle back. You start running and before long things begin to hurt: knees, feet, low back, etc. Next thing you know, you are back on the couch...This could all have been avoided if you stretched your hip flexors, activated your glutes, and at minimum went for a walk on a regular basis.
I often see individuals who say their goal is to be able to play with their kids. Let's think about that for a moment...how much is required to play with your child? Not a lot, just some simple movements. So today, make a committment to not be sedentary and just move! If you job entails sitting at a desk for 6-8 hours start by just standing up every 20-30 minutes and walking to the water cooler....today can be the day you start to move again!
Have an awesome day!
Posted on October 6, 2014 | Permalink
Tabata Protocol

Tabata
Be smart with exercise selection, incorporate all 3 planes of motion (Sagittal, Frontal, & Transverse) and try to include a balance of chest, back, shoulders, core, and legs. It is a short workout so in addition to the EPOC (Excess Post-exercise Oxygen Consumption) benefits, you should also strive to incorporate the entire body.
Posted on June 18, 2014 | Permalink
The Proper Protocol
To date there continues to be a lot of ACL rehabilitation research released. Most of which continues to prove the things that we as practitioners already know. Research is great, we definitely need it, but what about the practical application of that research? Are clinicians actually following the recommendations or are we continuing to take patients through the same ACL protocol that has been around for years. You know, the one they gave you when you got hired at the clinic that there are a million copies of in the file cabinet under “standard injury rehabilitation protocols for our practice”.
We know that the initial post op protocol is to decrease inflammation, activate knee extensors and flexors, and obtain full range of motion early. This is necessary but there is something missing….first, was it a contact or non-contact injury? More than likely it was non-contact (research shows that greater than 75% of ACL injuries are non-contact). Think about that for a minute………the individual missed out on a proper prevention protocol and as a result of muscle imbalances and movement compensations, sustained an ACL tear. Does that standard protocol that you are following take this into consideration? Probably not. And if you are a decent clinician, you probably begin to factor this in around week 12. Problem is, by that time you are almost out of visits authorized by the patient's insurance company (another issue that has many factors).
In my humble opinion, a proper protocol would include assessing the other factors and not spending 100% of efforts on the injured knee. After all, the goal is full function, right? The knee was not the original problem, it is the result of other problems that were not addressed. Many of which can be assessed with your handy goniometer (a very effective tool when used properly).What if the pelvis was anteriorly rotated, what if there is SI joint disfunction, what if dorsiflexion is very limited? How about we assess the LPHC, non affected knee, and bilateral ankle range of motion the first time you assess the injured knee. The amount of information gathered would be huge in determining why the injury occurred. This information could then be utilized to restore optimal range of motion and function of the whole body and not just the injured limb which was caused by faulty mechanics.
You did all that great work on the injured leg and it was the non-injured side that lead to the problem and you did not address it. Does that make sense? No, it does not. Yes, rehabilitation is designed to fix a problem but as practitioners we have a responsibility to prevent injury as well and the current protocol does not do that. Many times too often an athlete is returned to play and sustains a new injury. Then everyone says that “they came back too quick…”…….NOPE, the true problem just was not addressed. LOOK DEEPER!
Posted on June 13, 2014 | PermalinkA Letter to Athletic Trainers
Every year around March I post something related to our wonderful profession, 2014 will be no different. The time has come to stop whining about how you are addressed and be more concerned about how well you do your job. Do you know what your job is? Are you fully aware of your skill set? If I asked one hundred AT’s this question, I am sure all would say yes but I’ll bet the majority of them still treat injuries like it is 1991…taping ankles and stretching hamstrings. I am far from being the best but I have learned a few things over my 15 + years in the profession and it frightens me when I look at my twitter feed, the concern is not about being a better AT but being recognized as more than just a trainer. This has been a topic of discussion for years and I am sure it will continue to be for more to come but how about taking a different approach. How about actually going out there and helping individuals get better through proper technique learned from reading research and discussions with individuals who know how to fix problems instead of placing bandaids on injuries? Taping ankles does not prevent ankle sprains, you can teach a monkey to tape an ankle, fill a water cooler, and drive a gator.
Our skill set is very unique within the realm of allied health care but yet we do not take full advantage of it. We complain about lack of respect, job availability, and pay but we do nothing to separate ourselves and show our true worth. It amazes me that in a profession where applied techniques should rule, they do not and we lean more on the latest modalities, etc. I need a Hivamat, cold laser, Normatec, the old faithful e-stim and ultrasound. These devices have their place with acute issues but the majority of cases we manage are a result of overuse. I was fortunate enough to attend a great ATEP program which promoted independent thought, I was even more fortunate to work in pro sports for several years and learn from some of the best in the business. Both experiences helped shape the AT I am today but they also take the back seat to me understanding what my job description is and what I need to do to ensure that I make every effort to excel at it everyday. For those who may need it, here is a reminder as listed on the NATA’s website and in this document:
Athletic trainers (ATs) are healthcare professionals who collaborate with physicians. The services provided by ATs comprise prevention, emergency care, clinical diagnosis, therapeutic intervention and rehabilitation of injuries and medical conditions.
- Recreational, amateur, and professional athletes
- Individuals who have suffered musculoskeletal injuries
- Those seeking strength, conditioning, fitness, and performance enhancement
- Others delegated by the physician
Athletic trainers deliver rehabilitation services under a physician’s guidelines.
Guidelines are general directions and descriptions that lead to the final outcome, thereby allowing the athletic trainer to rely on clinical decision making in constructing the rehabilitation protocol. Protocol are rigid step-by-step instructions that are common in technical fields and do not allow flexibility and/or clinical decision making.
Athletic trainers function under a physician’s direction.
The terms "direction" and "supervision" mean two different things. Most importantly, supervision may require the on-site physical presence of the physician and that the physician examines each and every patient treated by an athletic trainer. Direction, on the other hand, requires contact and interaction, but not necessarily physical presence.
Lets break this down:
“Athletic trainers (ATs) are healthcare professionals who collaborate with physicians.”
If you operate independently this is more important than anything, you must establish a relationship with a physician, preferably an orthopedic. It validates your existence and if you are good at what you do you will get referrals. Without a physician it will be difficult to use many of your skills legally. Thank goodness for state licensure.
The services provided by ATs comprise prevention, emergency care, clinical diagnosis, therapeutic intervention and rehabilitation of injuries and medical conditions.
What is prevention? In my opinion for the AT, it should be defined as: reducing the risk of sport-related injury through early diagnosis and treatment; and recognition of limitations and rehabilitation potential. This definition encompasses everything but emergency care and certain medical conditions and if followed properly, truly reduces chance of injury. The key phrase in NATA’s definition of an AT though is “therapeutic intervention and rehabilitation of injuries”. Therapeutic intervention in my eyes is hands on care to achieve a desired outcome. Does taping an ankle fall within those guidelines? In my humble opinion, no, but measuring ankle dorsiflexion, assessing rear foot angle, and testing hip strength does (there's a lot of research on correlation between hip strength and ankle instability). Another example would be the unwritten rule of stretching hamstrings because a patient/client says they feel “tight” without proper assessment. More often than not, the hamstrings are synergistically dominant due to an anterior pelvic tilt and reciprocal inhibition of the glutes. This may cause one to say their hamstrings “feel tight” which they are, but they are elongated under tension as a result of misalignment of the pelvis, not short and contracted. In this case, it is more appropriate to stretch the hip flexors and activate the glutes. It is this type of evaluation that prevents injury; early diagnosis and recognition of the musculoskeletal warning signs, in other words, therapeutic intervention.
- Recreational, amateur, and professional athletes
- Individuals who have suffered musculoskeletal injuries
- Those seeking strength, conditioning, fitness, and performance enhancement
- Others delegated by the physician
As an athletic trainer you may be in either of the settings listed above, respect only comes to those that earn it. If you work with athletes and they are always in front of you with the same issue, there is something you are doing incorrectly. My patients range in age from 11 - 81 years and compete at levels from recreational to professional. The approach taken to treating those musculoskeletal injuries does not differ because of age, setting, or level of competition. For those individuals in a strength & conditioning/fitness/performance enhancement role, if you are not the busiest individual in your place of practice something is wrong. You have the skills to not only address fitness, but to also deal with any musculoskeletal issues…use that to your advantage. Assess your clients as if you are in the athletic training room and then put them on a plan to move better, their performance will increase. You may say, but I do this….do you really, or do you just tell people you do? If you properly diagnose and follow appropriate protocol, not diverting because you are bored with it or you think they have progressed when they have not, then great! But most do not fall within this category. A colleague recently posted a blog on sticking with your plan, it is worth a read. Click here.
I choose a soft science for my graduate education because I felt it would make me better at rehabilitation and I must say it does. We get so wrapped up in returning an individual to playing status that we overlook one of our main responsibilities which is to protect the athlete. If you do not fix the problem and only bandaid it, you are not protecting the athlete, you are just adding to the problem. There is substantial research out there to back this, I wrote a short blog on it a while back, it can be found here.
The ability to work under the direction of a physician is a great responsibility, one that must not be taken lightly. There are too many individuals who worked too hard to get this profession to its current level for it to be compromised by individuals who are just lazy and want everything handed to them. As I stated in the beginning, I do not claim to know it all and I never will simply because I learn something new everyday. Every patient is an opportunity for me to learn something different about how the musculoskeletal system works from a functional perspective. If you do not have a comprehensive understanding of functional anatomy, get on that ASAP! There was a huge factor left out of your A & P class that most overlook. The cadaver was prone or supine on a table, the class did not address how everything changes once the kinetic chain closes. You have to open your mind to a different way of thinking, you have the knowledge, just apply it!
Yusuf Boyd, M.S., ATC, LAT, CES, PES, CKTP
BIOMechaniks: Train the Mind and the Body will Follow
Posted on February 26, 2014 | PermalinkMove - Perform - Restore Week 1
Move Perform Restore Week 1 from BIOMechaniks on Vimeo.
Move Perform Restore Week 1
Posted on January 31, 2014 | PermalinkWhy Stress Proper Posture
Poor posture can slow a client’s progress simply by not allowing them the ability to move through a full range of motion, recruiting all muscles necessary and available to perform said exercise. Minimal muscle action also does not burn the same amount of calories as full recruitment. And lastly, poor posture with exercise can lead to injury which can keep the client from exercising all together which would be the biggest hindrance to their goal.
A proper movement assessment requires one to have a great understanding of anatomy and biomechanical function to look closely at the Human Movement System. The National Academy of Sports Medicine (NASM) has devised a structured way for health and fitness professionals to perform a proper movement assessment with the Overhead Squat Assessment (OHSA). The OHSA is "designed to assess dynamic flexibility, core strength, balance, and overall neuromuscular control" (1). There is evidence to support the use of transitional movement assessments such as the OHSA, which appears to be a reliable and valid measure of lower extremity movement patterns (1).
Taking the information observed in the OHSA and using it to design a program for an individual should be a minimal start to any exercise program. As stated above, if a client displays improper movement patterns and they are not addressed, exercising could lead to injury and keep them from exercising all together. Seeking out a health and fitness professional with the NASM credentials should be on your list when considering starting a new exercise regimen.
1. Clark, MA, Lucett, SC. NASM Essential of Corrective Exercise Training. 2011
BIOMechaniks: Train the mind and the body will follow
Variety, Balance, and Moderation – what do they mean?
You read magazine articles and hear it on the news: the key to a healthy lifestyle is moderation along with variety and balance. But what exactly does moderation mean? Does it mean a daily splurge, weekly splurge, or a monthly splurge? Or does it mean if you are eating healthy 80% of the time, the other 20% does not matter?
Moderation is the act of limiting or restraining certain things. Moderation combined with variety and balance does lead to a healthier lifestyle. Variety helps keep food interesting while giving your body the proper nutrients it needs. If you continue to eat the same foods day after day, you will become tired of those foods and more willing to make an unhealthy decision or splurge. Also, different colors of food provide the body with different nutrients. For example, red fruits and vegetables give the body lycopene and blue fruits and vegetables contain anthocyanins. Thus, a little variety in the diet helps “spice things up” while providing a full range of nutrients.
Balance refers to the balance of the food groups and portions consumed. It is important to eat all the food groups. Restricting a food group could lead to deficiencies of certain vitamins and minerals. Also, portion sizes should be balanced. A “handy” way of remembering what a cup looks like is using the size of your fist. One fist or cup is the proper serving of a fruit or vegetable and whole grains such as pastas and cereals.
Lastly, moderation is the ultimate key. As mentioned, it is limiting or restricting certain foods from your diet. Restricting food groups is bad but restricting foods such as candy, fried foods, or sugary beverages is beneficial to a healthy lifestyle. This could be a gradual change such as only drinking one soda a day compared to four, etc. As far as “splurges” are concerned, it differs from person to person. One person may need a small daily splurge such as a piece of dark chocolate but another person may want to look forward to that coffee drink from Starbucks once a week. It is important for you to find the balance in your life and stick with it. If you customize your diet plan to your needs and wants, you are more likely to stay on track and motivated than if you just copied a diet from someone else. It is your life and your health so remember to eat a variety of foods, balance portion sizes, and keep everything in moderation.
Stephanie Bailey, Dietetic Intern University of Memphis
Posted on April 25, 2012 | Permalink
Losing Weight While Training
Strict dieting is not recommended while endurance training as it can lead to fatigue and a decrease in energy. However, it is important to be at a healthy lean body weight for optimal performance. For elite athletes, the average male is 6-9% body fat and the average woman is 9-12% body fat. In order to lose one pound, 3,500 calories must be burned. Thus, for a weight loss of one pound per week that is 500 calories a day or 1,000 calories per day for 2 pounds of weight loss in one week. It is best to be aware of caloric intake without heavily restricting consumption. If you decrease your intake too much, you will become tired more easily. Weight loss will come if you are eating properly while working out. Also, as you begin to lose fat, you gain muscle. Muscle is leaner than fat but weighs more. As such, the number on the scale may not be moving as drastically as you would like, but you are becoming leaner as you build muscle while losing fat.
BIOMechaniks: Train the mind and the body will follow
Posted on March 20, 2012 | PermalinkHigh Calorie and High Protein Foods
Endurance Training requires a lot of calories and protein for optimal performance. So much so that it can be hard for athletes to consume an adequate amount of calories. Research shows that an inadequate intake can hurt performance and lead to a quicker fatigue. As such, consuming enough energy and nutrients is vital.
Energy dense or high calorie foods include granola bars, nuts and seeds, nut butters and dairy products containing fat such as cheese. It is best to eat throughout the day consuming 4-6 meals every few hours to ensure adequate energy intake.
An example of a 4,000 calorie a day diet looks like*:
Breakfast: 2 slices whole wheat toast with 2 tbsp. peanut butter
1 banana
2 egg omelet
1 glass milk (skim or soy)
Snack: 1 cup trail mix
Lunch: Turkey wrap
16 tortilla chips
½ cup hummus
Mixed fruit
Snack: 1 piece of fruit
1 granola bar
Workout: Honey, sports gel, or sports drink
Post workout: Smoothie: 1 scoop protein powder, 1 cup Greek yogurt, 1 cup mixed fruit
Dinner: 6 oz. grilled honey dijon chicken
1 whole wheat dinner roll
1 baked potato w/ 1 tbsp. butter
1 cup steamed, seasoned vegetables
Snack: 3 chocolate chip cookies
1 glass milk (skim or soy)
*Your meal plan does not have to follow this scenario, adjust it to fit your schedule and workout routine. If your calorie limit is less than 4,000 calories a day, make the portion sizes smaller. If it is greater than 4,000 calories a day, increase the portion sizes or add more snacks into the day.
Stephanie Bailey - Dietetic Intern - University of Memphis
BIOMechaniks: Train the mind and the body will follow
Posted on February 16, 2012 | PermalinkFluid Balance and Exercise
Proper hydration is important for both endurance and strength training exercise as it is critical to survival and athletic performance. It is best to hydrate before, during, and after exercise. The American College of Sports Medicine (ACSM) recommends 5-7 mL/kg of fluid from both food and liquid to be consumed before exercise. This standard is for the athlete that is already properly hydrated and recovered from the day before, but an additional 3-5 mL/kg is recommended in under-hydrated athletes.
During exercise, fluid loss occurs through sweat as the body maintains normal body temperature and cardiovascular function. Fluid loss is also affected by the exercise intensity and duration, environment temperature and humidity, gender, and clothing worn. Dehydration is defined as losing more than 2% of body weight in fluid loss. On average, individuals lose 0-2 L per hour of exercise.
Post-exercise it is recommended that the individual consume 125-150% of fluid lost (in body weight). Electrolytes should also be replaced after exercise along with fluids. Water is the best option for replacing fluids and sports drinks are only necessary if exercise exceeds one hour. Vegetable juice, soups, salty pretzels and trail mixes, and jerky are good examples of post-work snacks that contain adequate amounts of electrolytes to be replaced.
Stephanie Bailey - Dietetic Intern - University of Memphis
BIOMechaniks: Train the mind and the body will follow
Posted on January 16, 2012 | PermalinkAthletic Trainer vs Personal Trainer
With March fastly approaching I decided to take it upon myself as an Athletic Trainer to help educate the public on our profession. Ask any Athletic Trainer if they have ever been referred to as a personal trainer and I am sure 100% of them will say yes. This is one of the biggest misconceptions about our profession, the comparison to a personal trainer. An Athletic Trainer (ATC), as defined by the National Association of Athletic Trainers (NATA) is "a healthcare professional who collaborates with physicians to optimize activity and participation of patients and clients. Athletic training encompasses the prevention, diagnosis and intervention of emergency, acute and chronic medical conditions involving impairment, functional limitations and disabilities. While practice act oversight varies by state, athletic trainers practice under state statutes recognizing them as qualified health care professionals similar to physical therapists, occupational therapists and other health care professionals. More than 70 percent of certified athletic trainers hold at least a master’s degree. The independent Board of Certification Inc. (BOC) nationally certifies athletic trainers. Athletic trainers must pass an examination and hold an entry-level bachelor’s or master’s degree to become an athletic trainer. To retain certification, credential holders must obtain 75 hours of medically related continuing education credits every three years and adhere to Standards of Professional Practice. The BOC is accredited by the National Commission for Certifying Agencies." Athletic training is recognized by the American Medical Association (AMA) as a healthcare profession.
A personal trainer develops, monitors and changes an individual’s specific exercise program in a fitness or sports setting; some personal trainers also make nutrition recommendations. Personal trainers can earn credentials through a number of agencies and can work as fitness trainers without formal instruction or certification. A personal trainer may or may not have higher education in health sciences. They may or may not be required to obtain certification or state licensing, participate in continuing education or become certified by any one of numerous organizations that set varying education and practice requirements. Specifically, personal trainers assess fitness needs and design appropriate exercise regimens, work with clients to achieve fitness goals, help educate the public on the importance of physical activity, and work in health clubs, wellness centers and other locations
where fitness activities take place.
With this being fact, how can one associate an Athletic Trainer as the same as a personal trainer? Is it because we mainly work with athletes? No. Is it because we work in many different settings ranging from sports teams to health clubs to factories to physician offices and everything in between? Maybe...Or is it a lack of knowledge by the general public on the profession? Yes, in my opinion it is. So what do we do as Athletic Trainer's to help educate individuals on our profession? We take every opportunity that presents itself to let people know the difference and why it is a difference that they should not take so lightly.
If your kid is playing football and gets hit, it is the Athletic Trainer who evaluates them on the field to determine the severity of the injury and whether or not it is safe for them to return to play from a medical prospective, not a guess based on no knowledge. The Athletic Trainer is the first line of defense in the sports medicine circle. Our vast experience allows us to work in many settings and we deal with injuries of all types. Athletic trainers work in physician offices as physician extenders, in rural and urban hospitals, hospital emergency rooms, urgent and ambulatory care centers, military hospitals, physical therapy clinics, secondary schools, colleges/universities, youth leagues, commercial settings and professional sports teams. The skills of ATs have been sought and valued by sports medicine specialists and other physicians for more than 60 years. As the U.S. continues its focus on reducing the effects of obesity and other chronic diseases, it is important that people have access to health care professionals who can support lifelong, safe physical activity. Below are a few testimonials on the role Athletic Trainers play and how effective we are in all settings.
Testimonials from Employers and Friends of Athletic Trainers
Physicians, Hospitals and Clinics
“Athletic trainers are a committed, essential component to physicians delivering the highest standard of team medical care to the patients of the Andrews Institute. They know how to relate to the patient so his or her recovery is as quick as safely allowable, whether that person is a professional or youth athlete or just an average mom or dad.”
-- James Andrews, MD, Andrews Sports Medicine and Orthopedic Center, Birmingham, Ala.
“Athletic trainers help enhance a physician’s communication with patients by serving as another source of expert information that patients can absorb. Athletic trainers are a key part of our sports medicine service delivery model.”
-- John Xerogeanes, MD, Chief of Sports Medicine, Emory Orthopedics and Spine Center, Atlanta, Ga.
“I realized early on in my career that ATs are the only health care professionals who devote their entire education and professional lives to taking care of active people. My patients experience excellent outcomes as a result of therapy provided by ATs. My patients love working with them. ATs are a value added service to my practice. I could not do without them.”
-- Thomas D. Kohl, MD, medical director, family practice physician; Director, Sports Medicine, Comprehensive Athletic Treatment Center, Wyomissing, Pa.
Legislators and Regulators
“As a state legislator concerned with health policy, affordable and accessible health care for all people is my primary concern. We must look for innovative solutions to providing health care because of the increasing shortages of nurses and other health care workers. One of the best ways to deliver health care services in the community is to better utilize certified athletic trainers. Athletic trainers are multi-skilled health care professionals who provide a unique combination of injury and illness treatment and rehabilitation with a substantial dose of injury prevention and general wellness.”
-- Former Representative Jerry Krummel, Oregon House of Representatives, District 26
Occupational and Industrial Setting
“Our company has had a certified athletic trainer on site since 2000 and since that time we have recognized the tremendous upside in the tangible and intangible benefits of this addition, including a savings of more than $245,000 in just 2002 alone in health care-related expenditures. We have also experienced a decrease of 67 percent for health care costs related to the low back. Additionally, our days away from work have decreased by 60 percent in the last three years. In the industrial setting, these results can be best accomplished by an individual with the medical knowledge and training of an athletic trainer. We wouldn’t have it any other way and will continue this program for the long term.”
-- James E. Marotz, DO, corporate medical director at Appleton Papers, Appleton, Wis.
Some of the info contained in this blog was taken from the NATA's website and documents "The FACTS about Athletic Trainers" and "Athletic Trainers - Not 'Trainers'".
BIOMechaniks: Train the mind and the body will follow
To Play Or Not To Play
Given the recent reactions to Jay Cutler’s decision to discontinue participation in the NFC Championship game between the Green Bay Packers and the Chicago Bears because he suffered an injury, I thought I would share a little information on the psychological process, specifically, the pressure we place on athletes to play through pain and injury.
Sport Ethic
Since the early 90’s there has been a growing interest in athletic participation and how athletes are socialized into conforming to what is referred to as the “sport ethic.” This “sport ethic,” as defined by Hughes & Coakley (1991), refers to what many athletes consider to be the definition of an athlete. Specifically, they noted four beliefs in which athlete’s consider as the criteria to be considered an athlete, which are: “sacrificing for the game,” “striving for distinction,” “accepting risks and playing through pain,” and “refusing to accept limits in the pursuit of possibilities.” (p. 309) But from where do athletes receive the idea that pain and injury is a part of sport participation?
As noted by Nixon (1993, p. 188), the beliefs and values within sport convey the message to athletes that, “they ought to accept the risks, pain, and injuries in sport.” Taking risks and playing through pain is accepted by athletes as part of striving for distinction or simply, “the game.” Athletes are often told that they have to work hard if they want to make it to the next level. For those who abide by the sport ethic, working hard entails enduring pain and injury. However, Hughes & Coakley (1991) noted that not all athletes conform to the sport ethic. They speculated even more to say that those athletes who are susceptible to group pressures, low in self-esteem, and those who view sport as their only chance to make it are more likely to conform to the sport ethic. Hughes & Coakley (1991) also noted that these athletes are socialized by others within the sportsnet to embrace the sport ethic.
SportsNet
Within today’s sport culture athletes who accept the risks of sports participation and play through pain and injury are the ones who the media glorifies as being dedicated, or having what it takes to make it. Research has shown (Hughes & Coakley, 1991; Nixon, 1993; Curry, 1993; Young, White, & McTeer, 1994) that coaches will say that they do not expect their players to play injured but often motivate them to do so when they think it is necessary. When athletes refuse to accept to do so, they are often regarded as “not having what it takes” to make it to the next level. Some researchers (Nixon, 1994a; Young, White, & McTeer 1994) have noted that along with being socialized into thinking that pain and injury is a part of participation, male athletes are often told they are not “real” men if they cannot accept the risks of participation and play through pain and injury. Athletes often hear from their coaches, teammates, and the media, “No Pain, No Gain.” (Hughes & Coakley, 1991; Nixon, 1994b) The fact that coaches and journalists often stress the acceptance of playing through pain and injury and praise those who do, constitutes pain and injury as a normal part of sport participation. (Curry, 1993; Nixon, 1993; Nixon, 1994a; Young, White, & McTeer, 1994) Given this fact one can only wonder how coaches and Athletic Trainers work together in keeping athletes healthy, considering the fact that Athletic Trainers have a sole responsibility to protect and care for athletes.
REFERENCES
Curry, T. J. (1993). A Little pain Never Hurt Anyone: Athletic Career Socialization and the Normalization of Sports Injury.Symbolic Interaction, 16 (3), 273-290
Hughes, R. & Coakley, J. (1991). Positive Deviance Among Athletes: The Implications of Overconformity to the Sport Ethic.Sociology of Sport Journal, 8, 307-325.
Nixon, H. L. II (1993). Accepting the Risks of Pain and Injury in Sport: Mediated Cultural Influences on Playing Hurt.Sociology of Sport Journal, 10, 183-196.
Nixon, H. L. II (1994a). Coaches’ Views of Risk, Pain, and Injury in Sport, with Special Reference to Gender Differences.Sociology of Sport Journal, 11, 79-87.
Nixon, H. L. II (1994b, November). Social Pressure, Social Support, and help Seeking for Pain and Injuries in College Sports Networks. Journal of Sport & Social Issues, 18 (4), 340-355.
Young, K., White, P., & McTeer, W. (1994). Body Talk: Male Athlete Reflect on Sport, Injury, and Pain. Sociology of Sport journal, 11, 175-194.
BIOMechaniks: Train the mind and the body will follow
Posted on January 25, 2011 | Permalink
